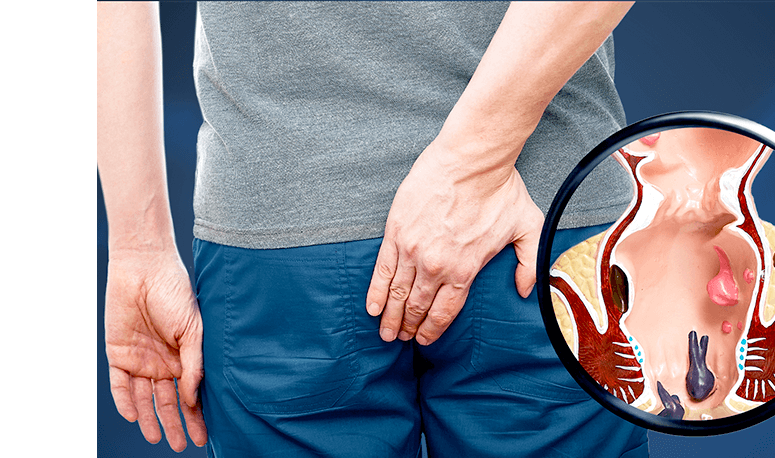
If you’ve been diagnosed with an anal fistula, it’s normal to feel a little anxious or uncertain about what comes next. Surgery in such a delicate area can sound intimidating, but the good news is that modern colorectal treatments are both safe and highly effective. These procedures aim to remove the fistula while maintaining your comfort and normal bowel function.
Two of the most common options your doctor might recommend are fistulotomy and fistulectomy. While both target the same issue, they differ in how the fistula tract is treated. Read on to understand how each procedure works, when it’s typically advised, and what factors your doctor considers when choosing the best option for you.
What Is Fistulotomy?
A fistulotomy is one of the most widely performed and trusted methods for anal fistulas repair in Singapore. The procedure involves carefully opening the fistula tract to allow it to drain and heal naturally from the inside out. By doing so, it removes the infection pathway and encourages healthy tissue regeneration.
Key benefits of fistulotomy include:
- Lasting relief from pain, infection, and abscess formation
- Lower recurrence rates through complete tract healing
- Faster healing times compared to more invasive procedures
- Often completed as a single, definitive procedure
When Is Fistulotomy Recommended?
Your doctor may recommend a fistulotomy if your fistula is simple, single-channeled, and involves minimal sphincter muscle. It’s especially effective for external or superficial fistulas that don’t pass through large portions of the anal sphincter. If you’ve had prior abscess drainage or tried conservative measures without success, a fistulotomy can provide a more lasting solution. However, for complex or higher fistulas, alternative techniques such as seton placement, flap repair, or laser closure may be safer and more effective.
How Fistulotomy Is Performed
Depending on the fistula’s complexity, the procedure is carried out under local anaesthesia, sedation, or general anaesthesia. The surgeon makes a small incision along the fistula tract, opening it up to release infection and promote proper drainage. Any unhealthy tissue is removed, and the wound is usually left open to heal gradually — though in some cases, sutures may be used.
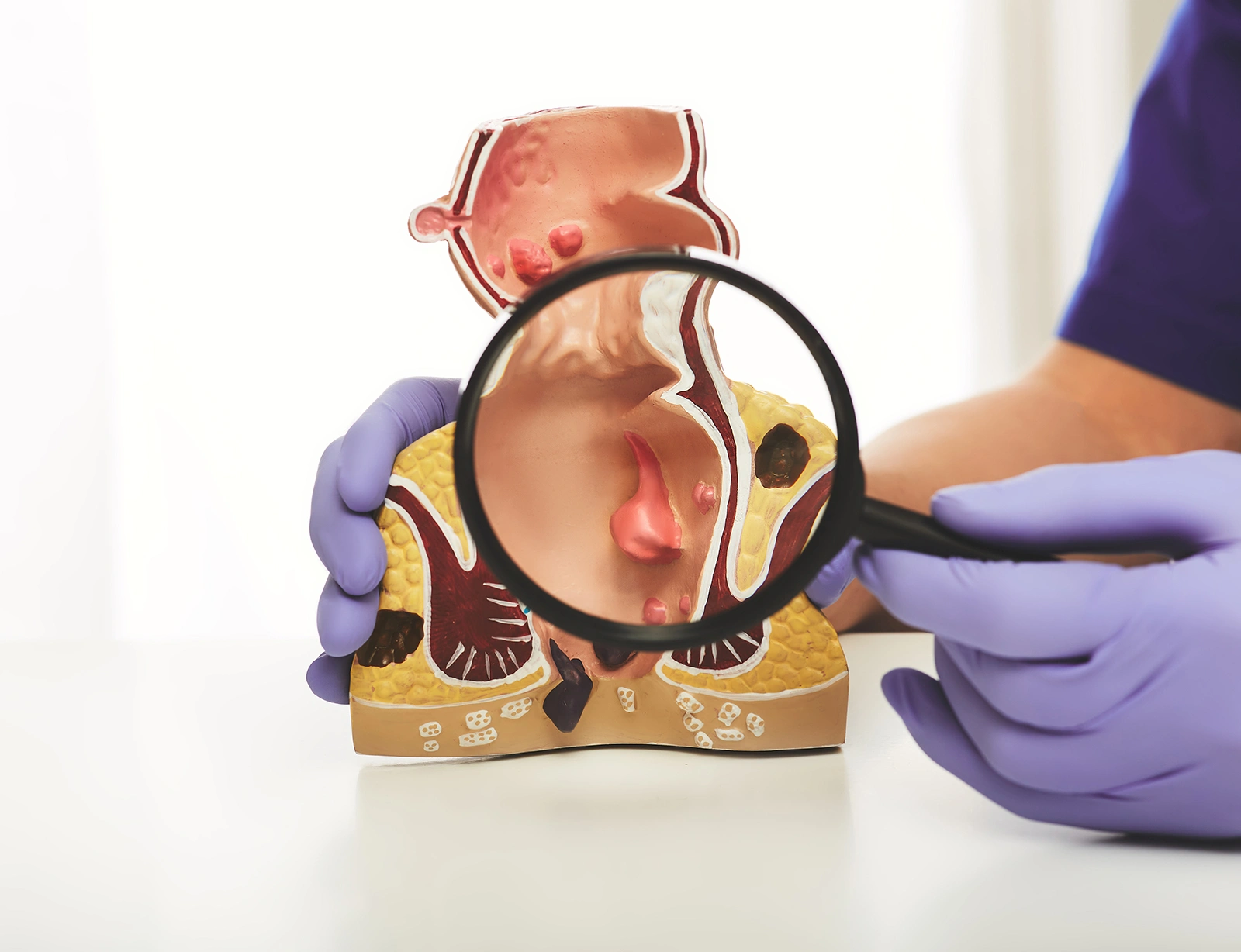
What Is a Fistulectomy?
A fistulectomy is a surgical procedure that involves the complete removal of an anal fistula and the surrounding infected tissue. Unlike fistulotomy, which only opens the fistula, a fistulectomy excises the entire fistula tract, leaving a wound that is left open to heal naturally.
Key benefits of fistulectomy include:
- Complete removal of the fistula and infected tissue
- Reduced recurrence, particularly for complex or high fistulas
- Effective when unresponsive to previous treatments
- Preserves sphincter function by targeting only affected areas
When Is Fistulectomy Recommended?
Fistulectomy is generally advised for complex, deep, or recurrent fistulas, especially when other treatments haven’t been successful. It’s also suitable for patients with multiple tracts or those who’ve experienced repeated infections. If your surgeon determines that a simple opening of the tract might not be enough, a fistulectomy ensures that all infected tissue is removed in one procedure, promoting more thorough healing.
How Is Fistulectomy Done?
The procedure is performed under general anaesthesia in a surgical setting. The surgeon first inserts a probe to trace the tract’s path from the internal opening in the anal canal to the external one on the skin. Once mapped, the entire tract and surrounding infected tissue are carefully removed.
Depending on the depth and size of the wound, it may be left open to heal naturally or closed with stitches. The wound is typically packed with gauze to support healing and prevent infection. The operation usually takes 30 to 60 minutes, and patients are observed after surgery before being discharged with follow-up instructions.
How Do Doctors Decide Which Procedure to Use?
There’s no one-size-fits-all approach when it comes to anal fistula repair. The recommended treatment is based on a comprehensive evaluation of the following factors:
- Fistula Complexity: Simple tracts usually respond well to fistulotomy, while deeper or branching ones may require a fistulectomy.
- Fistula Location: Advanced imaging tools such as MRI scans or endoanal ultrasound help pinpoint the tract’s course and minimise risk to the sphincter.
- Patient’s Surgical History: A history of recurrent or failed repairs may prompt the need for a more comprehensive removal through fistulectomy.
Ultimately, your treatment plan is a collaborative decision between you and your colorectal surgeon. Open communication and a clear understanding of your options can make the process far less daunting and help you approach surgery with confidence.
If you are experiencing symptoms of an anal fistula, schedule a consultation for anal fistula repair in Singapore to explore the best treatment options for your condition. Contact our clinic today to book an appointment.

Dr Dennis Koh
Medical Director & Senior Consultant Surgeon
B Med Sci (Nottingham), MBBS (Nottingham)
MMed (Surgery), FRCS (Edinburgh), FAMS
Dr Dennis Koh is an MOH-accredited and experienced colorectal surgeon skilled in anal fistula treatment; and currently the Medical Director at Colorectal Practice.
Dr Koh strives to provide a customized treatment plan for each patient, which allows for better outcomes. He also honed his skills in proctology abRd in Geneva, bringing a more diverse touch to his practice.

Dr Sharon Koh Zhiling
Senior Consultant Surgeon
MBBS (Singapore), MMed (Surgery),
FRCS (Edinburgh), FAMS
Dr Sharon Koh is an experienced colorectal surgeon and the former Director of Endoscopy at Alexandra Health.
Dr Koh completed her fellowship at Cedars-Sinai Medical Centre in the US after being awarded the Academic Medicine Development Award by the National University Hospital.

Dr Pauleon Tan Enjiu
Senior Consultant Surgeon
MBBS (Singapore), MMed (Surgery),
FRCS (Edinburgh), FACS
Dr Pauleon Tan has served in public hospitals for over 15 years and is experienced in minimally invasive surgery and endoscopy.
Dr Tan undertook advanced colorectal surgical training at Japan’s Saitama International Medical Center after being awarded the Ministry of Health – Health Manpower Development Plan (HMDP) Award.

