Many patients hesitate to seek treatment for anal fistula, often worried about painful recovery or the risk of losing bowel control. Fortunately, modern medicine now offers a range of minimally invasive anal fistula treatments designed to make recovery smoother and preserve anal function.
Unlike traditional fistulotomy, today’s approaches aim to seal or close the fistula tract from within, reducing trauma to surrounding tissues. Recovery times are typically shorter, and patients often experience less postoperative pain and faster returns to daily life.
Keep reading to learn more about the various minimally invasive options available, how they work, and what to consider when choosing the right approach for your condition.
LIFT Procedure (Ligation of Intersphincteric Fistula Tract)
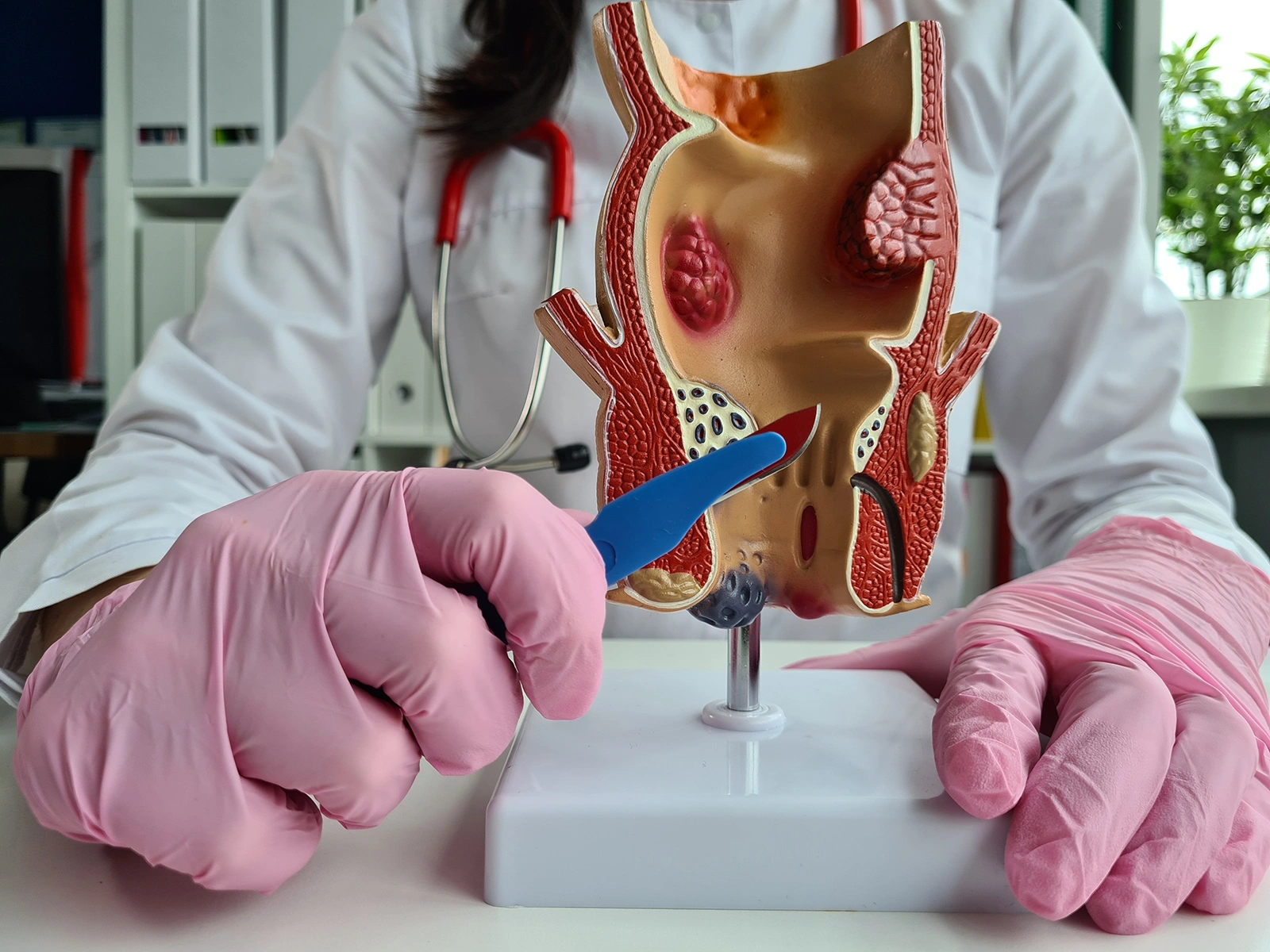
The LIFT procedure targets the fistula tract in the space between the internal and external sphincter muscles. During this operation, the surgeon carefully locates and ties off the tract, then closes the internal opening to prevent further infection or drainage.
Because the procedure is performed between the sphincter muscles rather than through them, it significantly reduces the risk of incontinence while still offering good success rates. The LIFT technique is also particularly useful for transsphincteric fistulas, which pass through both sphincter muscles. Patients generally experience less postoperative discomfort and can resume normal routines relatively quickly.
VAAFT (Video-Assisted Anal Fistula Treatment)
VAAFT uses a small endoscope to visually assess the fistula tract from the inside, allowing the surgeon to accurately map the tract, cauterise it and close the internal opening under direct vision. This approach offers both diagnostic accuracy and minimally invasive treatment in one procedure.
As the tract is treated internally, external incisions are minimal, which helps promote quicker recovery and reduced scarring. VAAFT is often recommended for more complex or recurrent fistulas, where precise identification of the tract’s route is critical. However, it requires specialised equipment and expertise to ensure optimal results.
FiLaC (Fistula Laser Closure)
The FiLaC technique makes use of a fine radial laser fibre that emits controlled energy to gently ablate and seal the fistula tract. When the laser is withdrawn, the tract collapses and closes, allowing surrounding tissue to remain intact. This method is known for reduced postoperative pain, minimal tissue disruption, and shorter recovery time compared to traditional surgery.
FiLaC is best suited for simple or moderately complex fistulas and is particularly appealing to patients seeking a less invasive option with minimal scarring.
Seton Placement (Cutting and Non-cutting Setons)
Seton placement involves inserting a fine thread-like material through the fistula tract to aid in healing and infection control. A cutting seton works gradually, tightening over time to divide the sphincter muscle safely while allowing the tract to heal behind it, reducing the risk of abscess recurrence. In contrast, a non-cutting seton keeps the tract open to allow drainage, which is especially useful in cases with active infection. It can also serve as a temporary measure before performing a definitive repair.
Setons are a flexible and widely used approach, particularly for complex or multi-branch fistulas, where immediate closure may not be advisable.
Fibrin Glue or Bioprosthetic Plugs
For patients who prefer a non-surgical or biological option, fibrin glue and bioprosthetic plugs offer alternatives that promote healing without cutting or removing tissue.
Fibrin glue is injected into the tract to seal it, while bioprosthetic plugs made from natural collagen are inserted to close the opening and encourage tissue regeneration. Both methods are quick, low-risk, and preserve sphincter integrity. However, it’s worth noting that recurrence rates may be higher compared to other surgical techniques, so these options are generally best reserved for select cases or patients prioritising minimal intervention.
Advantages of Minimally Invasive Techniques
Minimally invasive procedures for anal fistula offer several benefits over traditional fistulotomy. These include:
- Less postoperative pain and discomfort
- Lower risk of sphincter damage, which helps reduce the chance of incontinence
- Shorter downtime and quicker return to daily activities
- Outpatient or day surgery options, so hospital stays are often unnecessary
Patient Selection and Considerations
Not every case of anal fistula can be managed using minimally invasive techniques. Careful evaluation by a colorectal surgeon is vital to determine the most appropriate treatment. Factors that influence this decision include:
- Fistula type and complexity: Simple tracts often respond better to minimally invasive options, while extensive or branching ones may require combined approaches.
- Presence of infection: Active abscesses usually need to be drained before any repair can be attempted.
- Previous surgical history: Past interventions can affect anatomy and influence treatment planning.
- Continence preservation: Protecting anal sphincter control remains a top priority in all procedures.
- General health and suitability for anaesthesia: Patient fitness impacts both safety and recovery.
- Commitment to postoperative care: Proper wound care and follow-up visits are key to ensuring good outcomes.
Minimally invasive techniques offer effective alternatives to traditional surgery, especially for those seeking reduced discomfort and better sphincter function preservation. At our clinic, Dr Dennis Koh, Dr Sharon Koh, and Dr Pauleon Tan take a comprehensive approach to care, assessing each case in detail before recommending the most suitable option.
If you’re experiencing ongoing pain, drainage, or swelling, don’t wait for symptoms to worsen. Call us at 6262 1226 to schedule a consultation and explore the most suitable treatment for your recovery.

Dr Dennis Koh
Medical Director & Senior Consultant Surgeon
B Med Sci (Nottingham), MBBS (Nottingham)
MMed (Surgery), FRCS (Edinburgh), FAMS
Dr Dennis Koh is an MOH-accredited and experienced colorectal surgeon skilled in anal fistula treatment; and currently the Medical Director at Colorectal Practice.
Dr Koh strives to provide a customized treatment plan for each patient, which allows for better outcomes. He also honed his skills in proctology abRd in Geneva, bringing a more diverse touch to his practice.

Dr Sharon Koh Zhiling
Senior Consultant Surgeon
MBBS (Singapore), MMed (Surgery),
FRCS (Edinburgh), FAMS
Dr Sharon Koh is an experienced colorectal surgeon and the former Director of Endoscopy at Alexandra Health.
Dr Koh completed her fellowship at Cedars-Sinai Medical Centre in the US after being awarded the Academic Medicine Development Award by the National University Hospital.

Dr Pauleon Tan Enjiu
Senior Consultant Surgeon
MBBS (Singapore), MMed (Surgery),
FRCS (Edinburgh), FACS
Dr Pauleon Tan has served in public hospitals for over 15 years and is experienced in minimally invasive surgery and endoscopy.
Dr Tan undertook advanced colorectal surgical training at Japan’s Saitama International Medical Center after being awarded the Ministry of Health – Health Manpower Development Plan (HMDP) Award.

